Featured News - Current News - Archived News - News Categories
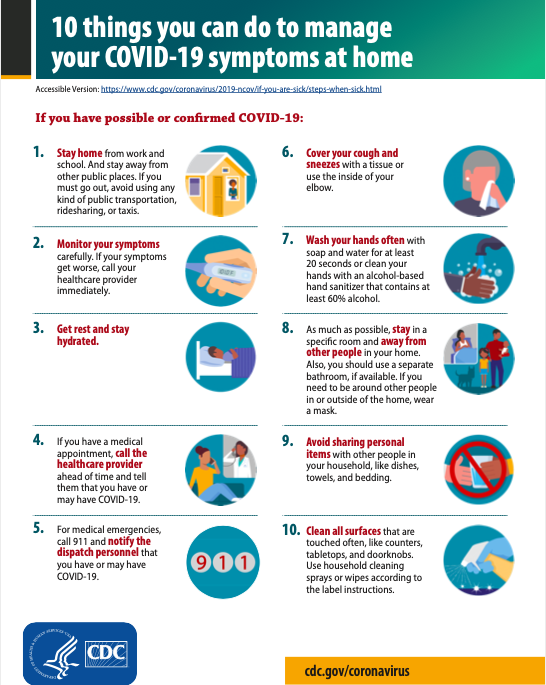
Gives insight on mask-wearing, possible transmission from air, surfaces
Q&A by Joshua Maloni
GM/Managing Editor
At the start of this year, how many people would’ve guessed wearing a mask, socially distancing and washing hands would become the new kale, exercise or hot yoga?
It’s been said there was no playbook for the coronavirus. Instead, health experts and elected leaders had to come up with better practices on the fly, test those ideas with research, and see what worked best to limit the viral spread and keep people healthy.
Last spring, these individuals spent copious amounts of time studying and discussing how businesses and restaurants could reopen. They then spent the summer months preparing for fall, and determining how students could return to a classroom setting.
Indeed, much of the conversation centered on the aforementioned preventative safety measures. Both the Centers for Disease Control and the National Institute of Allergy and Infectious Diseases – led by Director Dr. Anthony Fauci – agreed washing hands, wearing a mask and socially distancing would effectively limit the spread of COVID-19 and prevent virus-related deaths.
But as fall crept in, a lot of the talk turned political, and it became more difficult to ascertain what should be done when winter arrives. Or what did we learn in the warmer months that could help us in the colder ones?
Per the numbers, Niagara County is doing an admirable job in keeping the number of infections low. As the percentage of new positive test cases in Western New York rose above 2.5% last week, Niagara County was under 2% each day. It was below 1% Tuesday. Gov. Andrew Cuomo has said the coronavirus is manageable up to a 1% infection rate.
Leading the charge locally is Public Health Director Daniel Stapleton. The Niagara County Department of Health has worked hand-in-hand with the Niagara County Legislature, municipalities and school districts in setting (and maintaining) safety guidelines.
Stapleton spoke with NFP on Monday, providing insight and clarity on what is known now, what happens next, and what residents can do to limit their exposure to the coronavirus.
An edited Q&A follows.

Public Health Director Daniel Stapleton
Q: The infection rate numbers have been a little higher, but I’d say Niagara County is still doing pretty well. The other metrics seem to be moving in a positive direction. How would you say Niagara County is doing overall today?
Dan Stapleton: I think compared to a lot of parts in our region, our state and our country, I think our numbers are looking good – favorable compared to those. Of course, we're not happy with the numbers. Nobody should be happy with the numbers. But we do believe that our numbers, comparatively, are much better.
We look at the positive cases. We have a lot of positive cases today. But we also look at the infection rate. And it's important for people to keep that in mind. And also, we look at the hospitalization rate – and hospitalization rate for us, we have two people in the hospital today with COVID.
I think if you know the numbers, you'll see that that's very favorable compared to just in our region, let alone the rest of the state.
Q: And that seems to have been the trend over the past few months. Why do you think Niagara County has done so much better than other areas in Western New York?
Dan Stapleton: I think other places in Western New York are all working hard and are doing a fantastic job. I think it's hard to know, but I think the public following the rules is a big part of that. I'm sure there are other reasons, but we've always had a very robust surveillance system here in Niagara County. We've done a lot of educating and we've always done it. And so, I think it's a combination of factors.
But I think it's true when I say that all of the regions and counties are working hard to do that. I think we all have different situations that impact us.
We've been fairly vigilant over the many years because we're an international border, so that makes us a little more cautious and vigilant. We have a lot of visitors. Typically, in a typical tourist season, we have a lot of visitors – you know, 8 million people from 24 different countries; those types of stats. So, I think we've always had to be very vigilant because of the number of risks that we have in our county.
And I just think that, thankfully, the public has taken it serious, and is continuing to keep up on this vigilance – even when it's difficult to continue to do that.

Q: What have we learned about mask-wearing in the past six months?
Dan Stapleton: I go to every single school. I've been to all the schools. We're doing rapid COVID testing in every school district. We have Wilson, Roy-Hart this weekend. Then we'll be following-up with the last one in Barker. So, so far, I go to schools, I see that the students are really good at wearing masks. Young people know what they need to do and they do it. I've been pleasantly surprised by, when I go through the schools, I see students there following the rules.
I wish I could get all of the students in college and in higher education doing the same thing, because we're seeing a little bit of a laxness in that population. That concerns me, because those numbers in the 20-somethings and 30-somethings, those numbers are increasing fairly quickly compared to all the rest of the age groups.
Q: Is mask-wearing more to benefit the other person than the individual mask-wearer? In other words, is it more to keep someone who may have coronavirus to keep their droplets to themselves, as opposed to just protecting the average person; because the average person wearing a mask, I mean, they're still breathing the air? So, how does that work?
Dan Stapleton: I think it is. There's two parts of that answer.
The first one is, yes, we have people wear that so they don’t, if they are positive, they're not (spreading it).
First of all, they shouldn't be out in public, or they shouldn't be in close contact with people, regardless of whether they have a mask on or not. But yeah, it's to protect; it’s to keep the droplets and stop them from spreading the virus.
But for people who have a compromised immune system, the elderly, people who have a compromised immune system – whether it's chemo or whether it's chronic diseases that keep them from being able to be as healthy as they'd like – that protects them, too.
So, I think masks have dual uses. But of course, for the majority of us, it's to make sure that we don't spread anything in case we are asymptomatic. We don't have symptoms, but there's still a positive.
And secondary, like I said, it’s for people who have compromised immune systems – they’re being used, masks, to protect themselves.
It's funny, you know, years ago, even as recent as a few years ago, we would see in some countries that people were wearing masks, and the masks, when you would talk with individuals, is to protect others from the person wearing the mask. It's a good cultural phenomenon. But I think we see people now, people understanding that in our area, and doing what they need to do.
So, it depends on your situation, but it is a multiple approach for benefits.
Q: Wearing a mask, for me, it's something that I do faithfully when I go out. But I'm always curious about people that I see without a mask at public spaces, at gas pumps, entering or exiting a building. What do we know about the virus lingering in the air – and when these people come out of a public place and they take their mask off, are they putting others potentially at risk?
Dan Stapleton: A big part of the equation is the air exchange rate. The amount of fresh air. The breeze, if you will.
We believe – and we believe pretty strongly – that when you're out in public, out in the nonenclosed area, the risk is decreased significantly. I think that people who take it off, they should wait until they're out in the parking lot before they take them off.
A problem that I see, that maybe not everybody notices, is the amount of discarded masks that are out littering the communities. We shouldn't be putting the people who have to clean those up, we shouldn’t be putting them at risk. We should do the right thing and dispose of those things properly. It's disrespectful for people to throw their masks out and litter and expect that somebody else should have to be exposed to their masks.
That might just be a pet peeve of mine, but I see it way too often.
But back to your question, air exchange is a big part of that. Wait until you’re outside before you take them off.

Q: I don't hear a lot that's said these days about the danger of transmission from surfaces or other inanimate objects. Are we a little bit more comfortable that that's not as big a threat, or where do we stand with that?
Dan Stapleton: No. No. Hard services need to be cleaned. If you go to a school, there's nonstop cleaning of the surfaces, of the light switches, of the doorknobs, of the desks. You know, schools are taking this extremely serious; and they're making sure all that cleaning is happening throughout the day.
I don't think there's anything that I've seen that shows that that's a waste of time, or that it's being done too much.
Q: When we last spoke, we were going into the summer months and you said sunlight affects the half-life of the coronavirus. How does the cold affect it?
Dan Stapleton: My understanding, from what I've read and what I've heard anecdotally, is the cold, it's not impacted by that.
We've always believed that the flu, the seasonal flu, that that's impacted by that. We do see that the numbers decrease and the transmission decreases as weather gets warmer. It could because of the warm weather, but also because we're outside more.
Q: There's been a lot of talk about vaccines. What encourages you about the potential for a vaccine in the next couple of months?
Dan Stapleton: Well, I hear all different stories. I heard about a couple of studies that had to be paused to make sure that – somebody who came up with symptoms – that it wasn't related to the vaccine. But I do believe that there's a lot of vaccines that are nearing the end in terms of getting where they need to be with the safety and the testing. I'm optimistically hoping that we get some vaccine by the beginning of the year.
We had already started a month or two or three ago talking about our plans for mass-distribution clinics. I've talked to every school district superintendent about their availability, their building availability, for mass-vaccination clinics. That's something that we've been doing for months. And I've talked to every single school district superintendent about that, and they've all been very enthusiastic about allowing us to use that for mass-vaccination clinics.
As you probably know, we're using school district buildings for the rapid COVID testing that we're doing now. We've already been talking to them about mass-vaccination locations.
Stapleton said the NCDOH has identified other venues that could accommodate mass-distribution clinics.
We have a number of locations we talk with, and we have contracts with them, agreements with them. So, we're already starting to plan on prioritization of a vaccine.
Personally, I'm hoping we get the vaccine that only requires one dose, rather than one dose and then some more doses – another dose six months later or 60 days later, depending on the manufacturer. We're really hoping that we get the one-vaccine vaccination and not the ones that have to be done twice.
Q: A vaccine is not a cure. A vaccine is more to prevent people from getting this virus.
Dan Stapleton: Correct. It's not therapeutic. There's no therapeutic part of it. People are receiving therapeutic care now, when they get COVID, or some people are. So, no, this is not a cure. It's to prevent you from getting sick.
If you do get the disease, there’s also hope that – if it's similar to the seasonal flu – is that if you do get the disease, it'll lessen the symptoms and the duration of the illness. …
It's definitely not therapeutic, but we have other therapies that are being used for people with COVID right now.
Q: Any other words of wisdom for our audience as we enter the winter?
Dan Stapleton: Yeah, we want to make sure people get their seasonal flu vaccine. Vaccine is readily available. We want to make sure people get that vaccine. Because this is the way I'm looking at it: We want people to prevent the seasonal flu.
Someone who gets the flu, the seasonal flu, it weakens their immune system – it makes them more susceptible to other diseases. So, we want to make sure that they have a strong immune system, and that they don't get weakened by having a seasonal flu.
Secondary, we want people to continue to do the social distance, wearing masks, not going into crowds, only going out when they need to; those things that we’ve talked about all along.
People need to increase their vigilance, because now we have the seasonal flu. Our hope is that people who are taking this serious, they'll also reduce the risk of getting the seasonal flu by wearing their masks, social distancing, not going into crowds, mass gatherings – those types of things.
We follow Australia. Australia gets the strains of the seasonal flu before we do. Their season starts before ours. Right now, we're seeing a decreased infection rate of seasonal flu. And we believe that’s because probably people are getting vaccinated for the seasonal flu, but also they're following these guidelines more stringently than they would in a typical flu season.
So, we think that that's a positive sign, because we want to lessen the impact of getting a double-whammy from both COVID and the seasonal flu happening at the same time. That would be detrimental to the health of our populations that we serve. So, hopefully they'll be able to protect themselves and others by the seasonal flu shot. And then also follow the precautions that will make everyone safer.
For more information on the coronavirus, the Niagara County Department of Health is online at https://www.niagaracounty.com/Health.
Additional Resources:

Images courtesy of the Centers for Disease Control and Prevention